I'm posting some answers to the past year exam questions for all to review. Do comment should you notice any discrepancy or have anything to add. Also note that i have expanded on the explaination so i can squeeze in as much details as possible.
Qn : Mr Khoo has colo-rectal carcinoma stage III. He is admitted to your ward with wide spread metastasis. His pain is partially controlled with oral analgesics.
(b) Discuss the pain management strategies for Mr Khoo.
I always thought that metastasis automatically renders the individual into stage IV. Someone please confirm. Thanks. Below are my answers with the help of an open text.
*************************************
(a) Assessment strategies would include the following:
(i). Accurate classfication of Pain
Acute - Sudden onset, warns of imminent tissue damage
Chronic - Prolonged, complex and more difficult to control
* Note : Cancer pain may be chronic with acute flare ups
(ii) Use of the Pain Phenomenon as a guide:
1. Physiologic
2. Sensory
3. Affective
4. Cognitive
5. Behavioural
6. Socio-cultural
1. Physiological
- Associated with direct tumor involvement (eg. tumor pressing on nerves?) or cancer therapy (eg. Side effect of RT/chemo)
2. Sensory
- To note the following : * Location - Site, diffused/localised/generalized? *Intensity - As percieved by individual (how bad?) *Quality - Ask individual to describe nature of pain (Eg. Pulsating, aching, burning)
3. Affective
- To identify psychological factors that may contribute to pain - Eg. Deteriorating condition -> depression/anxiety -> more pain - Also note the personality traits of the individual (type 1/2) as this will also affect pain perception
4. Cognitive
- Highlights how pain affects the individual's thought processes
- Eg. more pain -> more anxiety -> depression - Individuals with positive attitudes reported less severe pain
5. Behavioural
- Identifies behaviour related to pain (Eg. level of activities) or intake of analgesic
* Note : Behavioural response to pain may or may not coincide with the individual's report to pain. Eg. The patient may report of a pain score of 8, but may still be able to continue with his ADLs.
6. Socio-cultural
- Include demographic, cultural, ethnic, spiritual and other related factors that influence the perception of pain
- Eg. It may be socially acceptable in some cultures to have outward bursts of emotion when experiencing pain
(iii) Use of a Comprehensive Assessment Tool
- Includes subjective (eg. verbalization of pain) and objective (what the nurse observes) data
Onset
Location
Description
Intensity (use of pain scales)
Aggravating & Relieving Factors
Previous treatment
Effect on pain on daily activities
Vital Signs
- Pain Scales (eg. Wong-Baker's Face, Numerical)
*************************************
(b) Firstly, the Nurse must understand that pain perception is a personal and subjective evaluation. Therefore, it is important nit to impose their own personal views which will be likely to obscure the assessment process. Continual pain assessment with the following guidelines should be beneficial:
1. Pharmacotherapy
2. Complimentary Therapies
3. Other Therapies
4. Role of the nurse
1. Pharmacotherapy
- Use of the WHO's 3 step Analgesic Ladder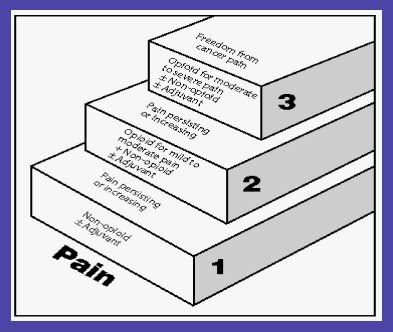
- Examples of Analgesics
(i) Non Opiods - Aspirin, Paracet, NSAIDs (naproxen, diclofenac, Ibuprofen)
(ii) Opiods - Weak - Codeine, Buprenorphine - Strong - Pethidine, Morphine, Fentanyl
- Examples of Adjuvants
(i) Anxiolytics - Diazepam
(ii) Antidepressants - Amitriptyline
(iii) Anticonvulsants - Sodium Valporate, Carbamezapine, Neurotin
(iv) Neuroleptics - Haloperidol
- Common Routes of Administration :
-> PO (preferred), S/C (bolus/continuous), PR, Transdermal, I/M, I/V, Epidural
* Rationale : The WHO's 3 step ladder aids in determining type & strength of analgesic required for effective pain relief.
* Nursing Responsibilities
(i) Medication must be given as presribed and on schedule (5 rights)
(ii) Dosage should be titrated to meet the individual's needs
(iii) Assess the need of adjuvant drug therapy
(iv) To observe and manage the side effects/complications of Opiods
- Eg. Constipation, N&V, Sedation, Mental CLouding, Respi depression, Urinary retention, xerostomia, pruritis, sleep disturbances
(2) Complimentary Therapy
(i) Psychological and Behavioural Therapy
- Eg. Distraction, Hypnosis, Relaxation, Guided Imagery, Music, Art, Muscle relaxation
(ii) Cutaneous Therapy
- Eg. Accupuncture, Massage, Transcutaneous Electrical Nerve Stimulation (TENS)
* Rationale : Improves coping strategies to deal with pain.
(3) Other Therapies
(i) Interventional
- Only 2-5% of Opiods direct to the CNS
- Individual may consider Nerve Blocks
(ii) Supportive Care
- Eg. Pastoral Care, Supportive Care
(iii) Anti-tumor Strategies
- Eg. Radiation, Chemotherapy, Surgery
(4) Role of the Nurse in Pain Management
(i) Believe in the patient's complaint of pain
(ii) Careful assessment
- detailed hx, physical & psychosocial assessment
(iii) Provide Psychological Support
- Encourage active participation in self care, verbalization of needs/feelings
- Include the family and social network (if possible)
(iv) Educator
- Teach effective coping strategies
- Discuss options of Pain management (safe and effective methods)
(v) Evaluation
- Individual's response to therapy, after initiation of treatment, at each new report of pain, and at suitable intervals after intervention
- Accurate documention of pain, S/E or treatment etc
* Rationale :
- Continual Assessment is important as it highlights the changes in pattern of pain, any new development or persistance in pain which will require either modification or change of current treatment.
- Failure to assess is the main cause if under treatment.